
Wound dehiscence occurs when the edges of a surgical incision reopen due to poor healing, infection, or excessive tension on the wound. It is a serious complication of both traumatic injuries and surgical procedures that can lead to increased pain, delayed healing, reoperation, hospital readmission, and higher treatment costs.
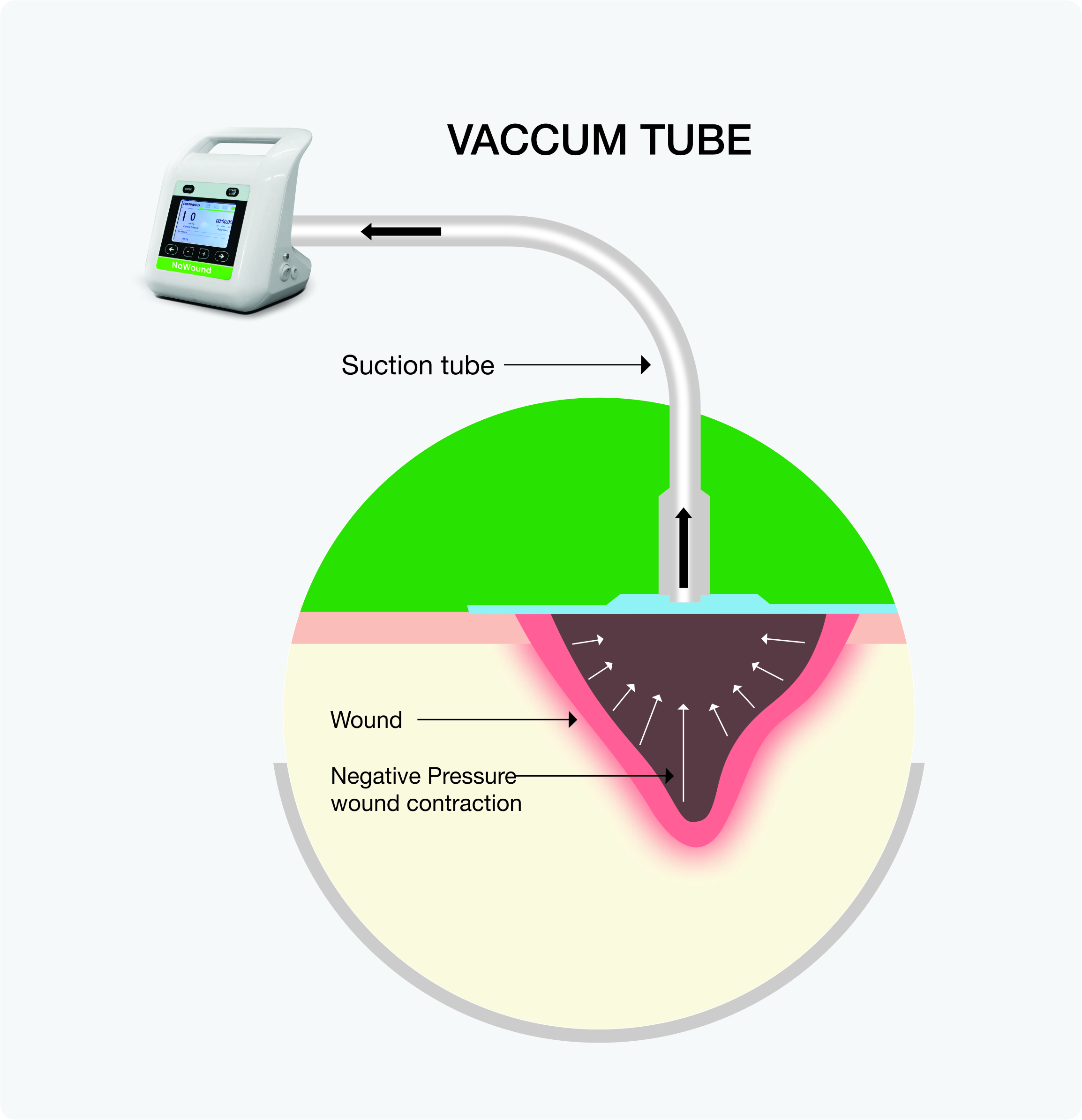
Negative pressure wound therapy (NPWT), also known as vacuum‐assisted closure (VAC), is a system that aids healing of these complex wounds by keeping the wound sterile, reducing tension across the incision, removing excess fluid, lowering the risk of infection, and promoting new tissue growth.
NPWT facilitates wound healing through several key mechanisms:
NPWT offers several advantages for traumatic and surgical dehiscence, including:
Faster Healing: Promotes tissue repair by creating an optimal healing environment.
Reduced Complications: Lowers infection risks and prevents fluid buildup (seromas).
Improved Comfort: Minimizes frequent dressing changes and reduces pain.
Controlled Healing: Provides consistent pressure for stable wound healing.
Cost-Effective: Shortens recovery time and reduces additional interventions.
Open Fractures/Exposed Tissue: Injuries with significant soft tissue damage and exposed bone or tendons are prone to contamination and infection. NPWT helps by removing debris, reducing swelling, and promoting blood flow for healing.
High Contamination/Infection Risk: Contaminated traumatic wounds with dead tissue or foreign bodies are at high risk of infection. NPWT helps by facilitating exudate removal and reducing the bacterial load.
Postoperative Wound Separation: NPWT helps bring edges together, promoting granulation tissue formation in surgical wounds that have partially or fully reopened.
Abdominal Dehiscence: NPWT stabilizes the wound, reduces edema, and protects the organs until closure in surgical wounds where the abdominal wall layers separate, often exposing organs.
Wound Preparation:
Dressing Application:
Sealing & Suction:
Monitoring:
NPWT is not suitable for all patients. Contraindications include:
Feature | NPWT | Traditional Wound Care |
Speed of Healing | Faster | Slower |
Risk of Infection | Lower | Higher |
Dressing changes | Less frequent | More Frequent |
Pain Level | Reduced | Higher |
Cost | Higher initially but more cost-efficient in the long term | Lower initially but higher long-term |
NPWT is recommended for dehisced wounds with excessive drainage, tissue loss, or poor healing. It is particularly useful when conventional wound care fails.
Healing time varies based on wound size, depth, and patient health, but NPWT often accelerates the process compared to traditional wound care.
Portable NPWT systems can be used at home, but proper training and follow-up with your care team are essential.
If the dressing becomes loose, it may compromise healing. If possible, reapply the seal or contact your healthcare provider for assistance.
If not properly managed, minor bleeding, skin irritation, and infection can occur. Regular monitoring and following medical guidelines minimize these risks.
NPWT can be used on infected dehisced wounds when combined with appropriate antibiotics and wound debridement. Your doctor will assess suitability based on the severity of the infection.
The optimal pressure setting typically ranges between 75-125 mmHg, depending on wound characteristics. Your healthcare provider will determine the best settings.
Dressings are typically changed every 2-3 days, but this may vary based on the wound and treatment plan.
NPWT can help reduce pain by minimizing swelling and stabilizing the wound environment, although some patients may initially experience mild discomfort.
You can continue moving around depending on the wound location and overall condition. The portable battery backup allows for 3-5 hours of mobility.
If you or a loved one is struggling with wound dehiscence, NPWT may be the solution you need. Consult a healthcare provider today to learn more about how NPWT can accelerate healing and improve wound outcomes.