
Chronic wounds can be challenging to treat due to prolonged healing time, increased risk of infections, high treatment costs, and complications such as necrosis and amputation
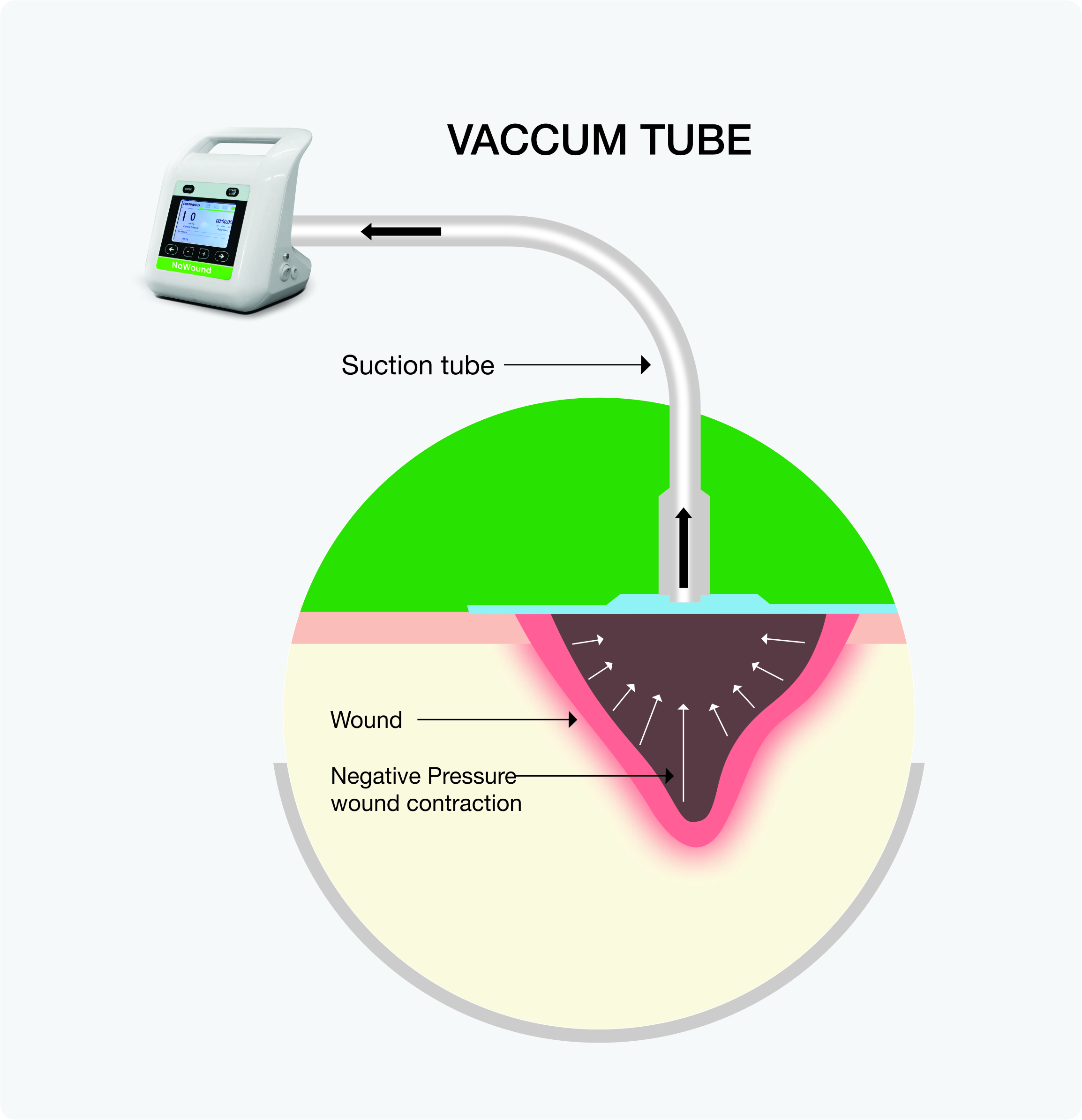
Negative Pressure Wound Therapy (NPWT) is an effective and non-invasive technique that applies controlled suction to the affected area to accelerate chronic wound healing. It helps remove excess fluid, reduce swelling, promote blood flow, and minimize infection risk, ensuring faster recovery.
NPWT accelerates wound healing by following mechanisms:
NPWT provides multiple benefits for chronic wounds, such as:
Foot ulceration is one of the most common complications of diabetes. It results from poor circulation and neuropathy in diabetic patients. The ulcers frequently become infected, causing progressive tissue necrosis and poor wound healing.
When to Use NPWT: NPWT is effective for complex DFUs, particularly those with significant tissue loss or after surgical debridement.
Considerations for use:
Pressure ulcers, also known as bedsores or pressure injuries, are lesions usually caused by intense or long‐term pressure, shear, or friction. They may be painful and infected and affect a patient’s quality of life. Pressure ulcers are more commonly seen in individuals who are immobile or have limited mobility.
NPWT reduces moisture, decreases bacterial load, and promotes granulation tissue. This helps reduce pain, pressure ulcer size, and severity, ensuring improved patient outcomes.
When to Use NPWT: For deep or severe pressure ulcers (Stage III or IV) with extensive tissue damage, undermining, or tunneling.
Considerations for use:
Pressure ulcers, also known as bedsores or pressure injuries, are lesions usually caused by intense or long‐term pressure, shear, or friction. They may be painful and infected and affect a patient’s quality of life. Pressure ulcers are more commonly seen in individuals who are immobile or have limited mobility.
NPWT reduces moisture, decreases bacterial load, and promotes granulation tissue. This helps reduce pain, pressure ulcer size, and severity, ensuring improved patient outcomes.
When to Use NPWT: For deep or severe pressure ulcers (Stage III or IV) with extensive tissue damage, undermining, or tunneling.
Considerations for use:
While NPWT is highly effective in wound management, it may not suit all patients. Some contraindications include:
| Feature | NPWT | Traditional Wound Care |
|---|---|---|
| Speed of Healing | Faster | Slower |
| Risk of Infection | Lower | Higher |
| Dressing changes | Less frequent | More Frequent |
| Pain Level | Reduced | Higher |
| Cost | Higher initially but more cost-efficient in the long term | Lower initially but higher long-term |
NPWT reduces swelling, removes bacteria, and gently pulls the wound edges together, ensuring a better environment for healing, especially for chronic wounds that do not respond to standard treatments.
The healing time varies depending on wound size, type, and underlying health conditions. While some wounds may heal within weeks, others, especially large, deep, or infected wounds, may require months of therapy. Your physician will monitor the progress and adjust the treatment plan as needed.
Some discomfort may occur, especially during dressing changes. Your doctor may adjust your treatment or suggest some medications to manage pain.
NPWT is safe for most, but not all, wounds. It should not be used on wounds with untreated infections, exposed blood vessels, or cancer in the wound bed. Consult a doctor to determine if NPWT is right for you.
NPWT dressings are typically changed every 2-3 days, but this can vary depending on the wound and the amount of fluid removed.
Depending on the wound location and overall condition, you can generally continue to move around. The portable battery backup on the NPWT device allows for 3-5 hours of mobility.
The waterproof dressing allows you to shower or wash while receiving NPWT, as long as the dressing isn’t soaked.
NPWT alarms will beep and flash orange if there’s a problem (like a leak or low battery). The screen will show the issue. Your care team will explain what triggers them and how to fix them.Some discomfort may occur, especially during dressing changes. Your doctor may adjust your treatment or suggest some medications to manage pain.
NPWT costs vary depending on the device, wound size, and treatment duration.
NPWT provides significant benefits for chronic wounds, including faster healing, infection control, and reduced hospitalization. Consult a wound care specialist to determine if it suits your condition.